Corneal Transplantation
The cornea is the clear front “window” of the eye, like the crystal of a wristwatch, transmitting light to the interior of the eye allowing us to see clearly. Corneal injury, disease, or hereditary conditions can cause clouding, distortion, and scarring. Corneal clouding, like frost on a glass windowpane, blocks the clear passage of light to the back of the eye, reducing sight.
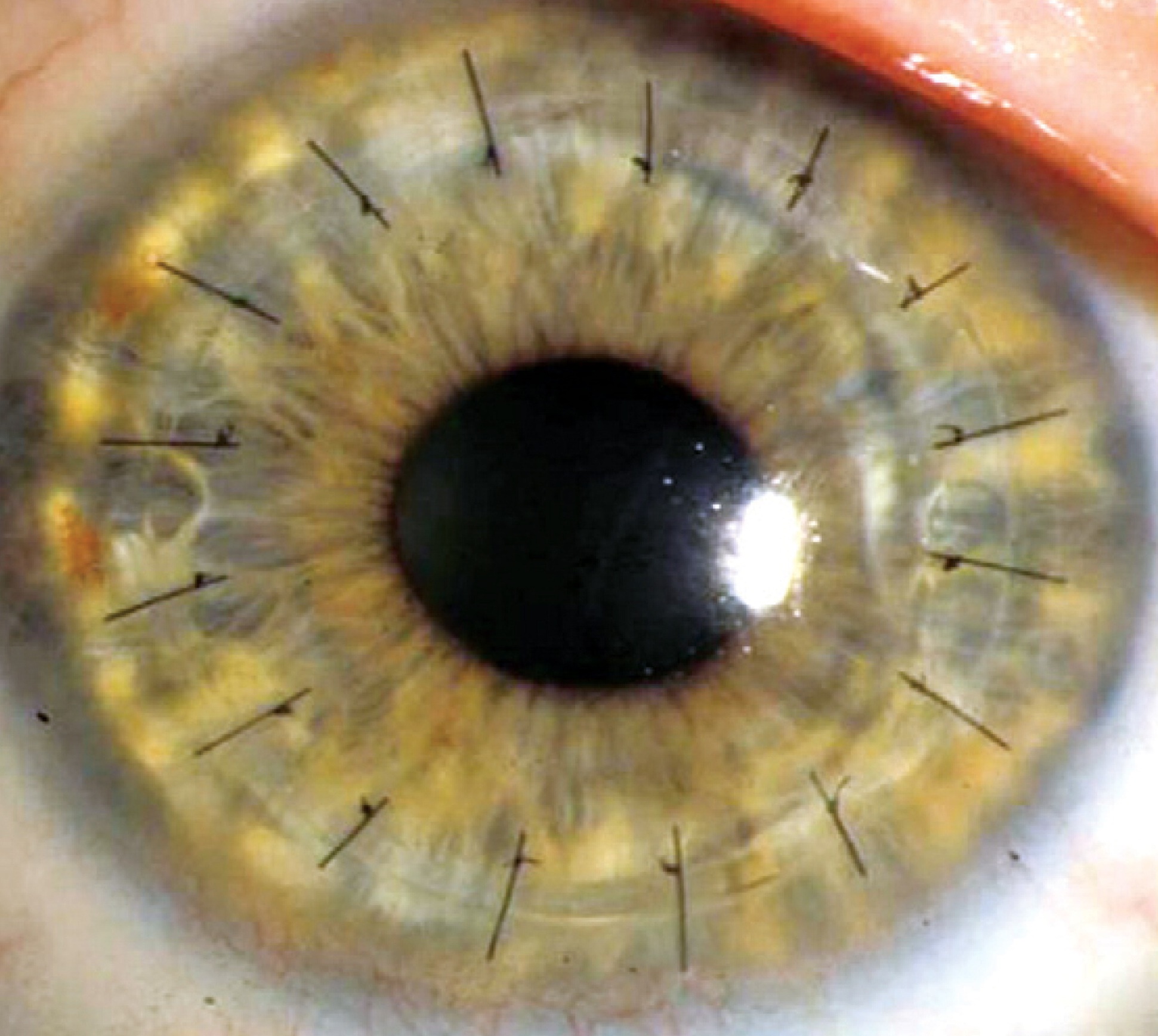
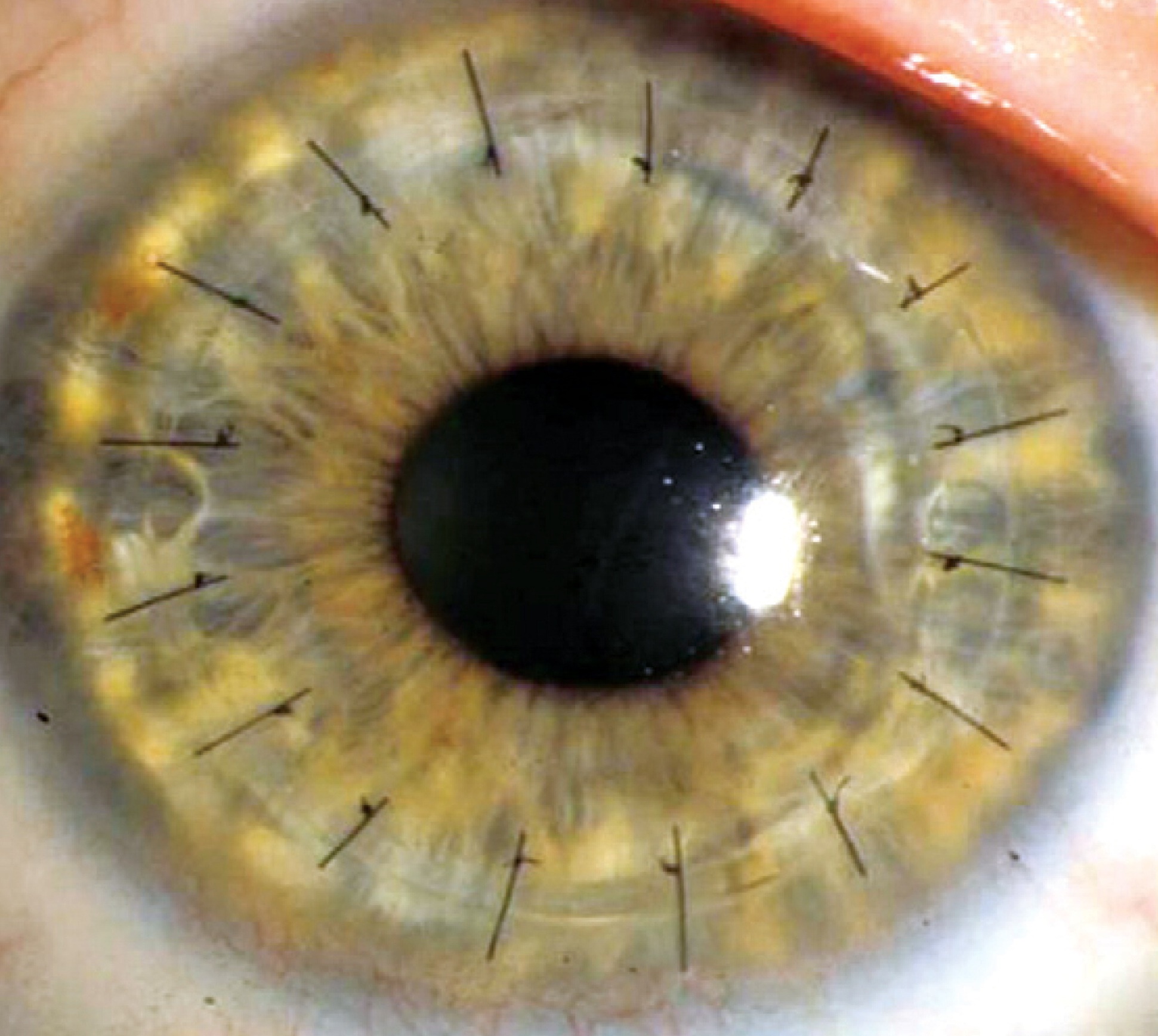
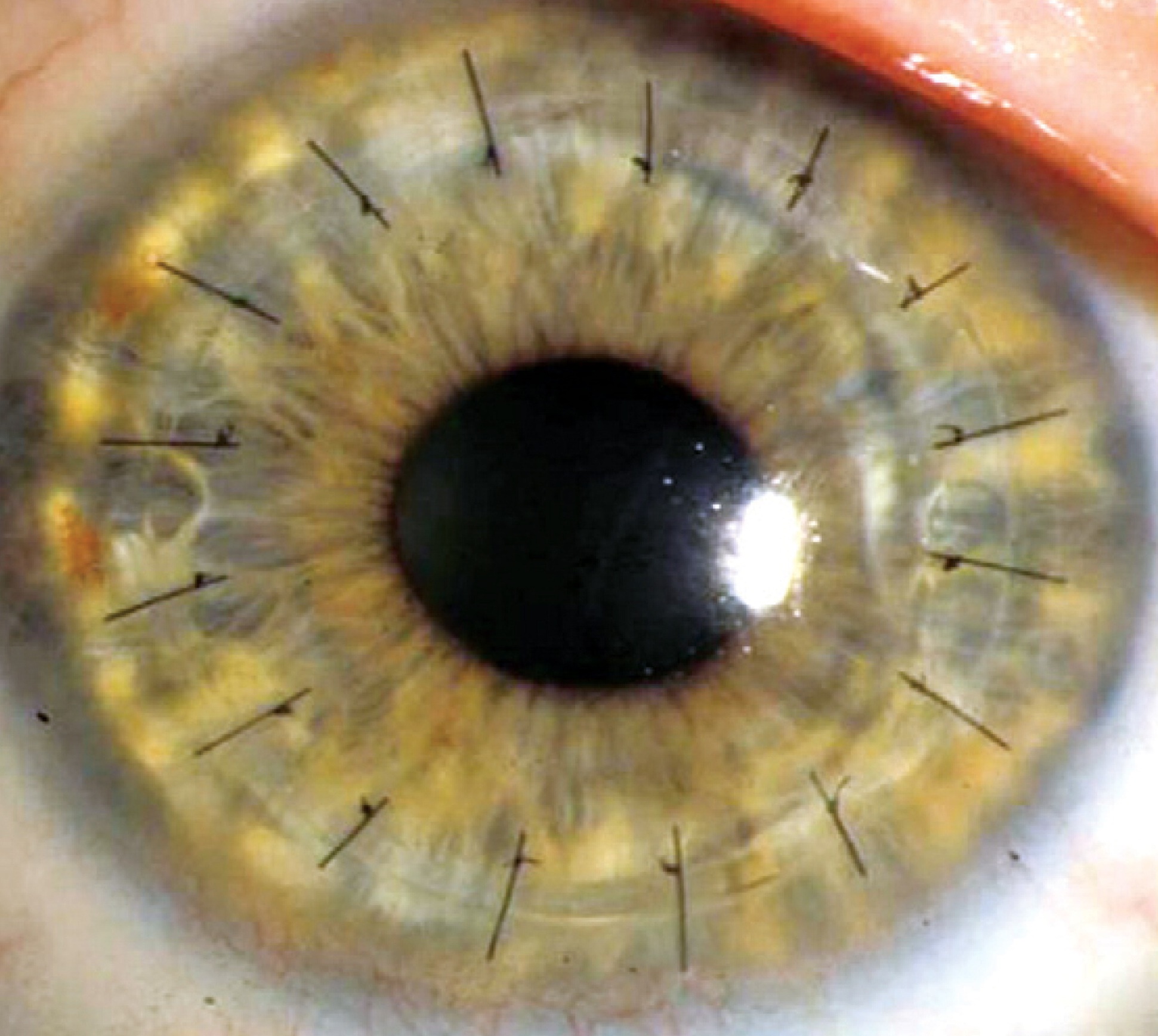
If the cornea becomes cloudy, the only way to restore sight is to replace or transplant the cornea. A corneal transplant is the removal of the diseased central portion of your cornea, and replacement of that tissue with a clear or clouded donor cornea. Corneal transplantation is the most successful of all tissue transplants. An estimated 40,000 corneal transplants are done each year in the United States. The success rate depends on the cause of the clouding. For example, corneal transplants for degeneration following cataract surgery and those for keratoconus both have high success rates, while corneal transplants for chemical burns have lower success rates.












The donor cornea is received through the eye bank from a person who has recently passed away. All tissue is tested to avoid transmitting the AIDS virus, and Hepatitis B and C from the donor to the recipient. Strict screening criteria must be met before tissue qualifies for transplantation.
Most patients have surgery on an outpatient basis and go home within several hours. The actual surgery takes between 30 and 45 minutes, and is usually done under a local anesthetic. You will be given medication for sedation while your eye is completely numbed. You will be awake but relaxed throughout the procedure. A sterile drape will be placed over your other eye. During surgery you will be unable to move, blink or see out of your eye (faint shadows or dim light may be seen). After surgery, specific precautions will be reviewed. We will provide you with specific instruction on how and when to use your medications.
NEW DSAEK: PARTIAL THICKNESS, NEAR-SUTURELESS CORNEAL TRASPLANTS


DSAEK (Descemet Stripping Automated Endothelial Keratoplasty) is a corneal transplant technique where the unhealthy, diseased, posterior portion of a patient’s cornea is removed and replaced with healthy donor tissue obtained from the eye bank. Unlike conventional corneal transplant surgery (penetrating keratoplasty or PK), the DSAEK procedure utilizes a much smaller surgical incision and requires no corneal sutures. The donor cornea is placed in the eye folded and is then gently unfolded using an air bubble to aid in attaching the donor tissue to the patient’s own cornea.


DSAEK is especially indicated for patients with Fuchs dystrophy and other situations where the cornea is clear but limited by unhealthy endothelial cells. With this nearly sutureless technique, astigmatism is nearly eliminated, there Is less risk of stich-related infection or vascularization, the globe remains structurally sound, graft rejection is less likely and full functional vision returns within weeks to months instead of months to years. DSAEK has become the standard of care for treating Fuchs’ dystrophy and postcataract corneal clouding. It also may be valuable in some patients with a failed PK.
ADVANCED TRANSPLANTATION – BOSTON KPRO
While many people can be helped by “traditional” corneal transplantation, in some cases such transplantation is hopeless, or nearly so. The Boston Keratoprothesis (Kpro) can be used after previous transplant failure, or when such a transplant would be unlikely to succeed, such as after a chemical injury to the eye. This procedure is designed to help patients whose conditions are the most difficult to treat.
The Boston Kpro has been under development since the 1960s and has been progressively refined since then. Significant advancements in both design and in understanding of factors critical to long term success of this prosthetic device (prevention of infection, management of co-existing glaucoma and control of inflammation) have boosted the use of this device to over 1000 cases annually in the United States. Over 13,000 KPros have been implanted since the device was made available to surgeons.
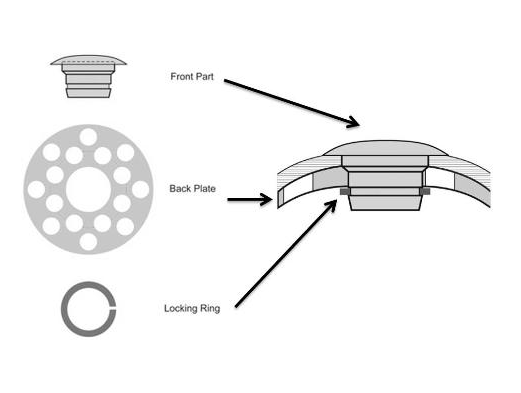
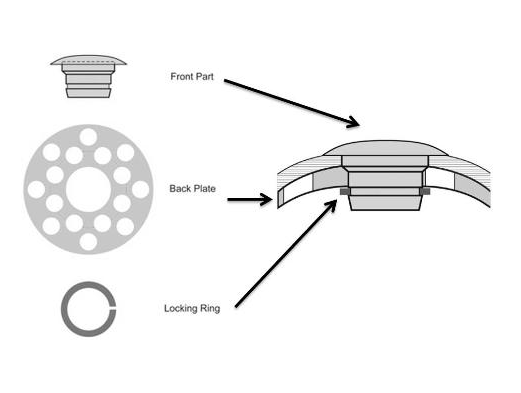
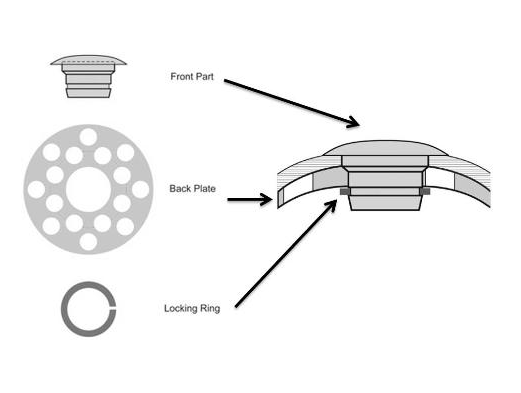
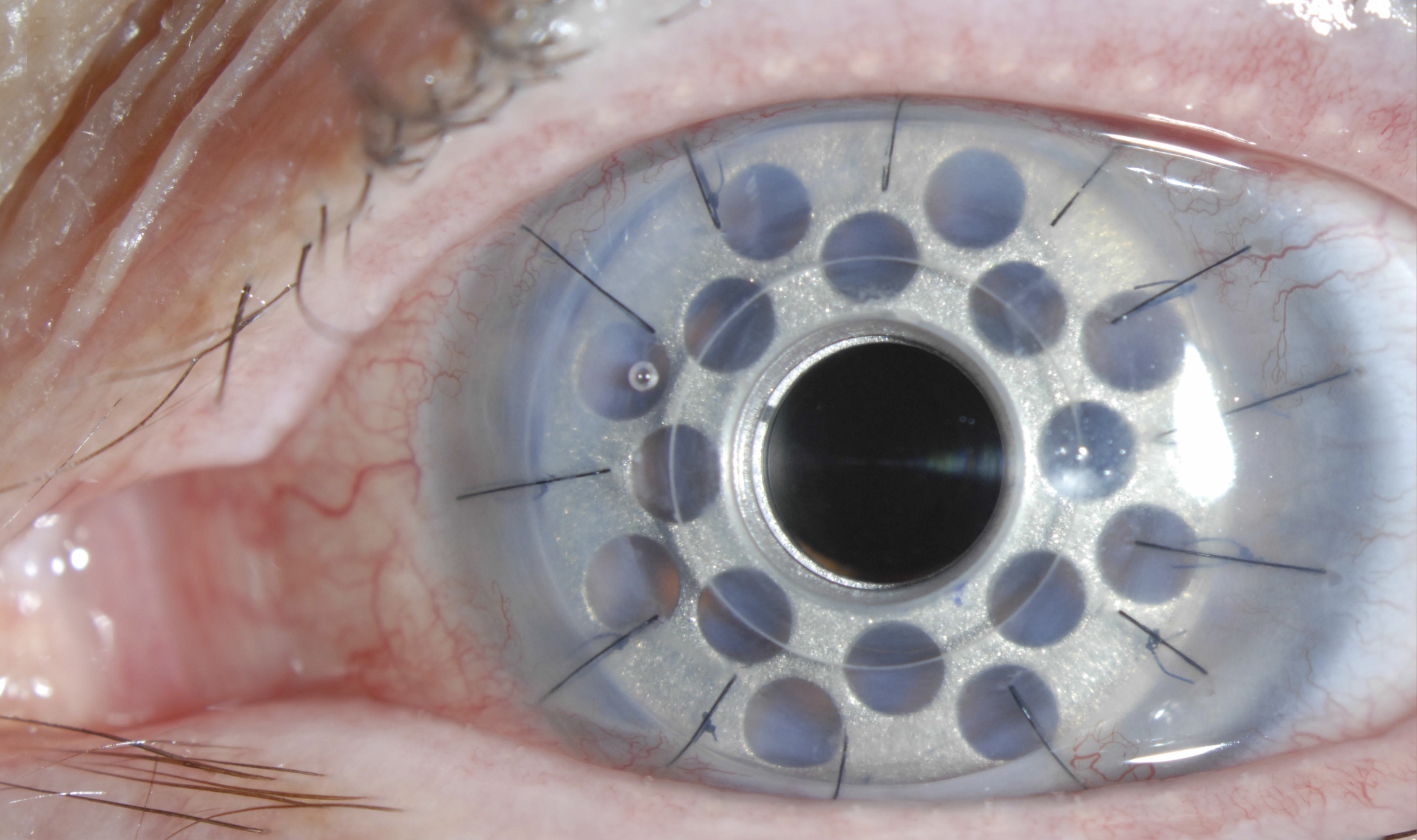
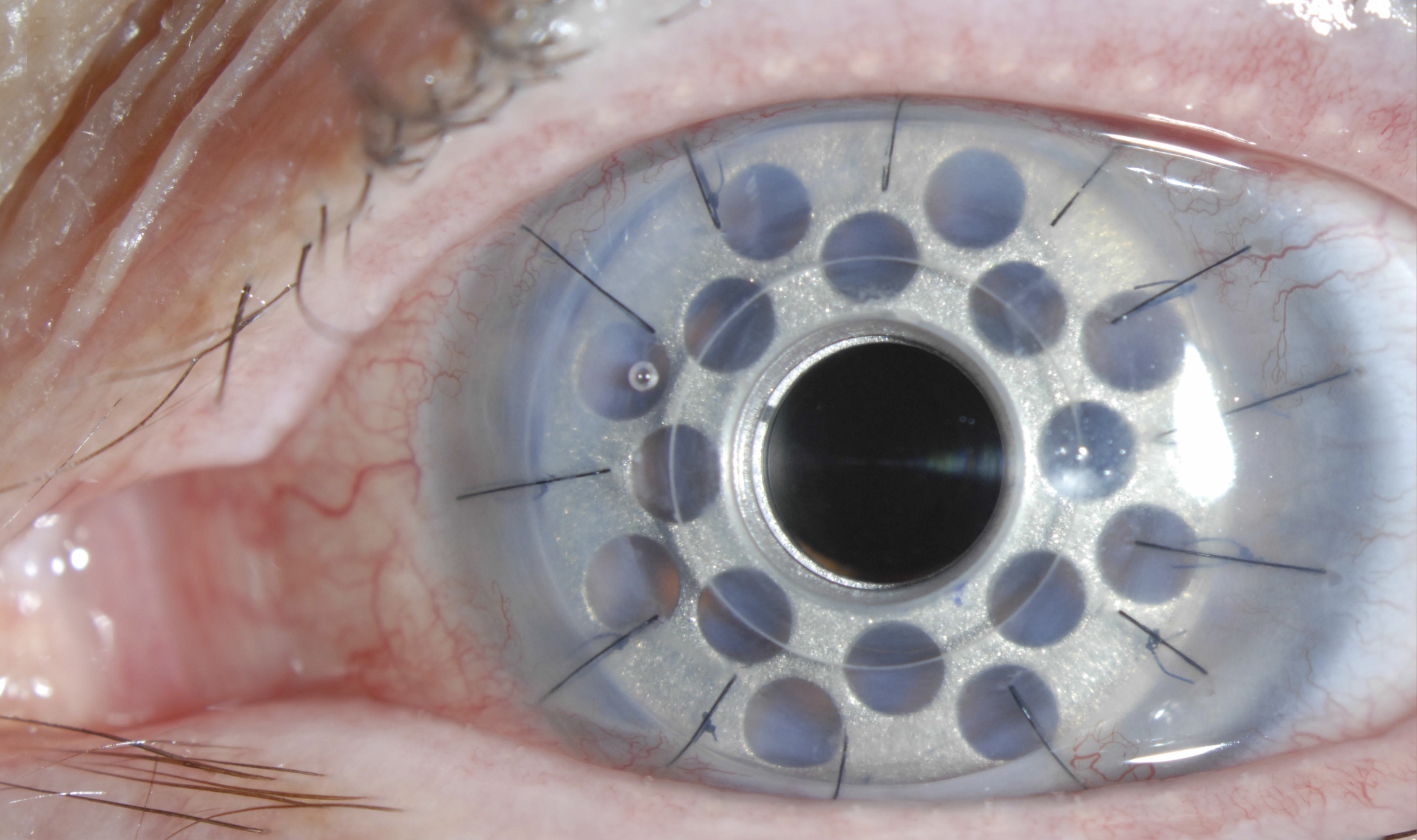
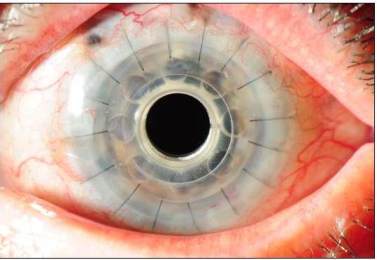
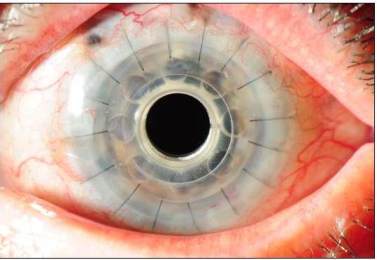
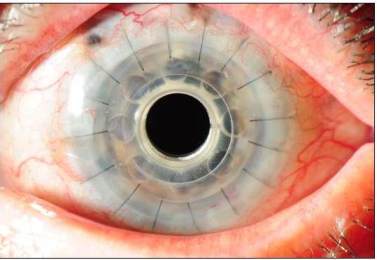
The keratoprosthesis is made of two pieces (see diagram) – a clear plastic front plate and a back plate (either plastic or titanium) – that form a “collar button” shape when assembled together with donor corneal tissue. The assembled device is sutured into the patient’s eye, just like a traditional corneal transplant. The special materials used allows nutrients to enter the eye more effectively than previous designs.
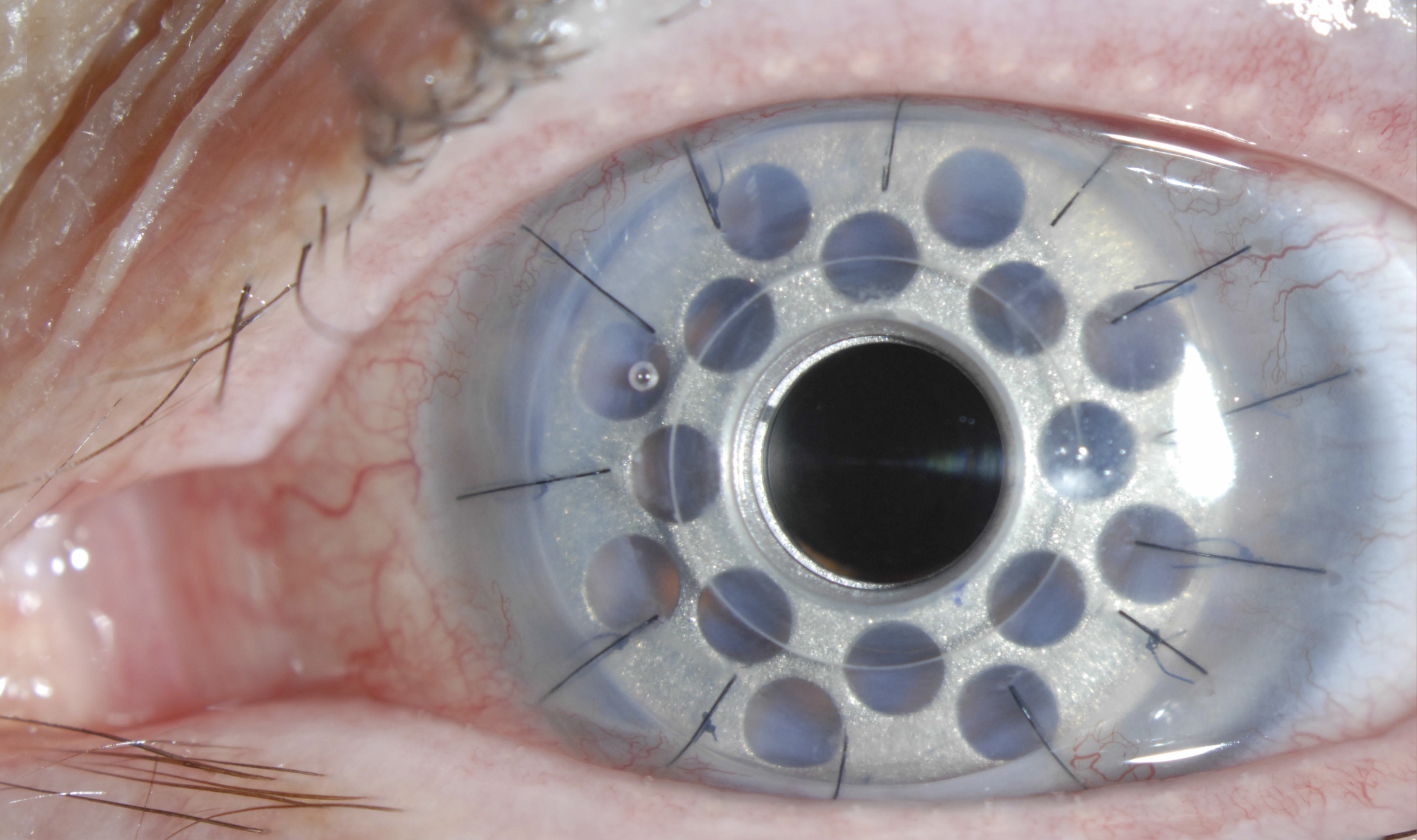
Dr. Tauber trained at the Massachusetts Eye and Ear Infirmary with Dr. Dohlman, who developed the keratoprosthesis and personally supervised refinements of the device over three decades. Dr. Tauber trained personally with Dr. Dohlman and has performed over 130 surgeries with the Boston Kpro. For patients who have been told there is no hope to regain their vision due to corneal blindness, the Boston Kpro offers hope.