Keratoconus


Keratoconus is a non-inflammatory eye condition in which the shape of the cornea becomes distorted. The cornea is a clear structure that covers the front of the eye and allows light to enter the eye. In a healthy eye, the cornea curves like a dome. In an eye with keratoconus, the center of the cornea slowly thins and bulges, so that it sags and has a cone shape (see illustration).
Keratoconus occurs in 50 to 230 per 100,000 population. Despite a great deal of experience with keratoconus, the cause is still unknown. Some believe that keratoconus is a degenerative condition while others believe it is genetic in origin. It is known that 13% of patients have a relative with keratoconus. It occurs more frequently in patients with allergies or asthma and is associated with forceful eye rubbing. This excessive eye rubbing may weaken the structural strength of the cornea, allowing bulging to occur or progress.
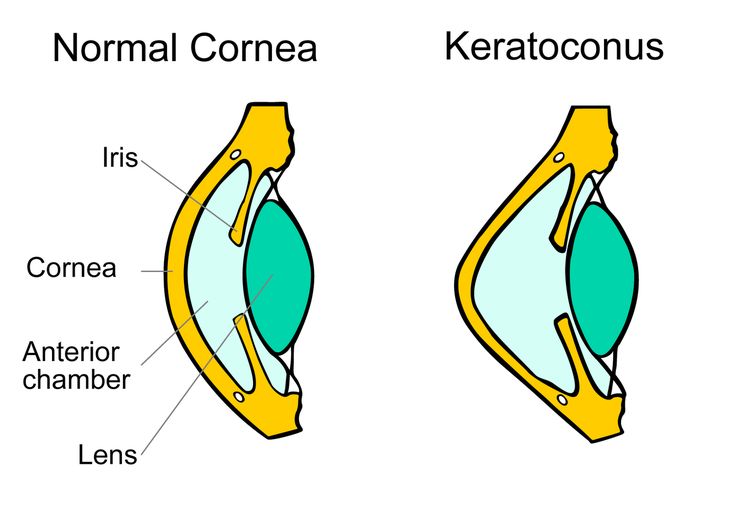
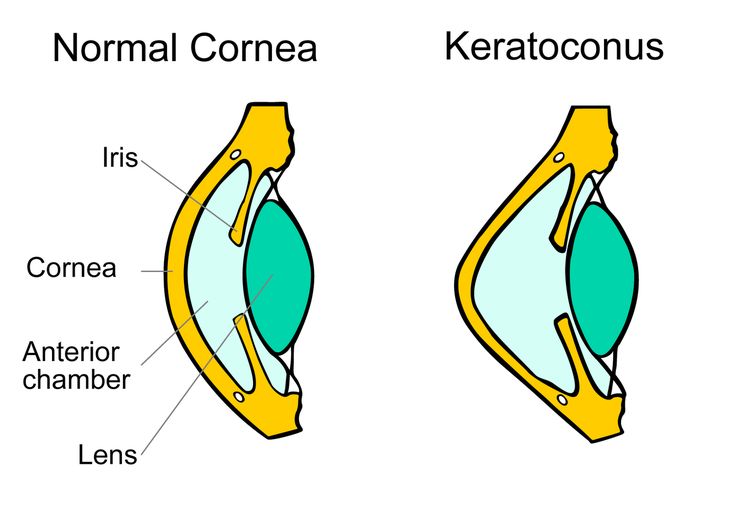
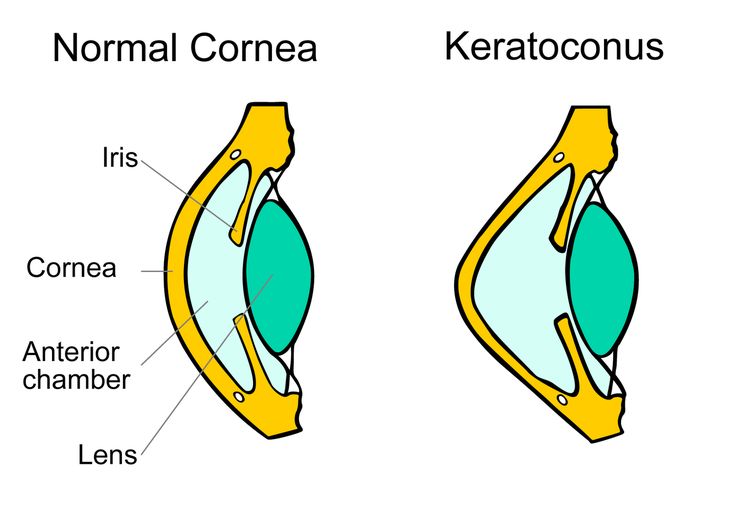
Symptoms of keratoconus usually start in the teenage years and may progress for the next 10 to 20 years. The early symptoms include decreased vision and fluctuating nearsightedness. Blurring and distortion of vision are common. Wrinkles and scars may also form on a keratoconus cornea.
Keratoconus is usually discovered when a patient sees an ophthalmologist or optometrist because of decreased vision or frequently changing eye glass prescriptions. The diagnosis of keratoconus can be made through careful examination of the eye. Often, computerized mapping of the corneal shape (corneal topography) is necessary to confirm the diagnosis.



People with keratoconus may suffer from decreased vision in two ways:
From distortion of the cornea: Seeing through a misshapen cornea is like taking pictures with a camera whose lens has an irregular (not smooth) surface (is like looking through a warped windshield). Parts of the field of vision are in focus and parts are out of focus. This visual problem is called irregular astigmatism.
From scarring or swelling of the cornea: Seeing through a scarred or swollen cornea is like taking pictures with a camera with a dirty or cloudy lens (is like looking through a dirty windshield). The picture or vision is blurred or hazy.
Keratoconus TREATMENT



Corneal Crosslinking



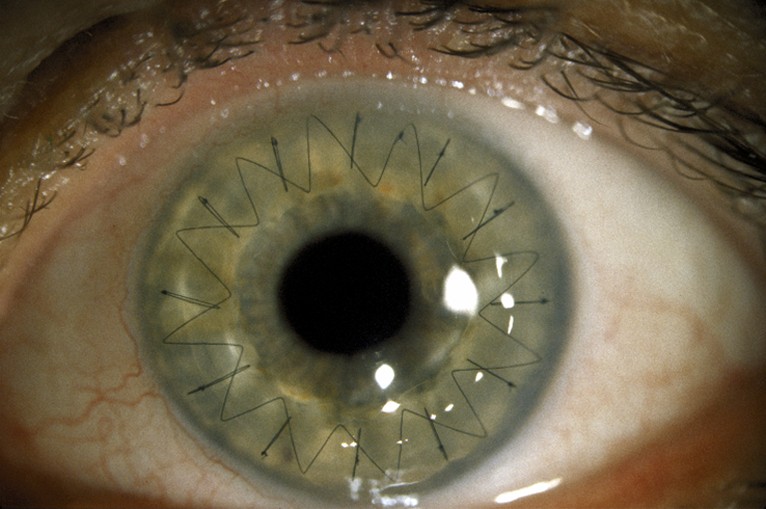
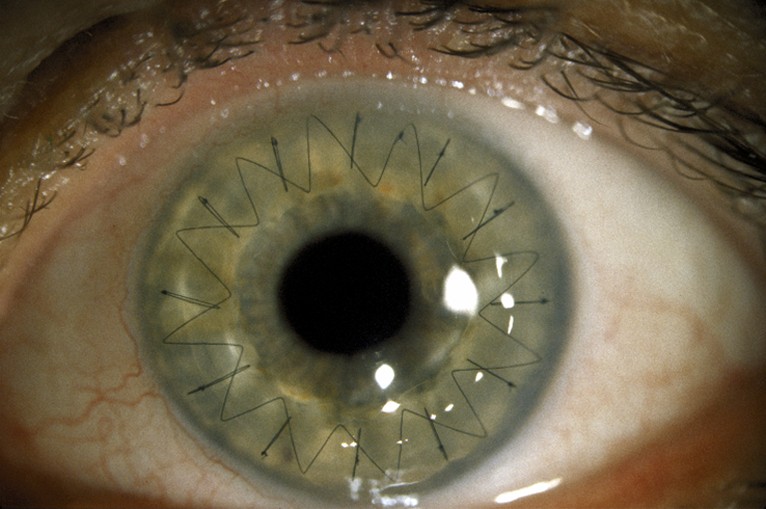
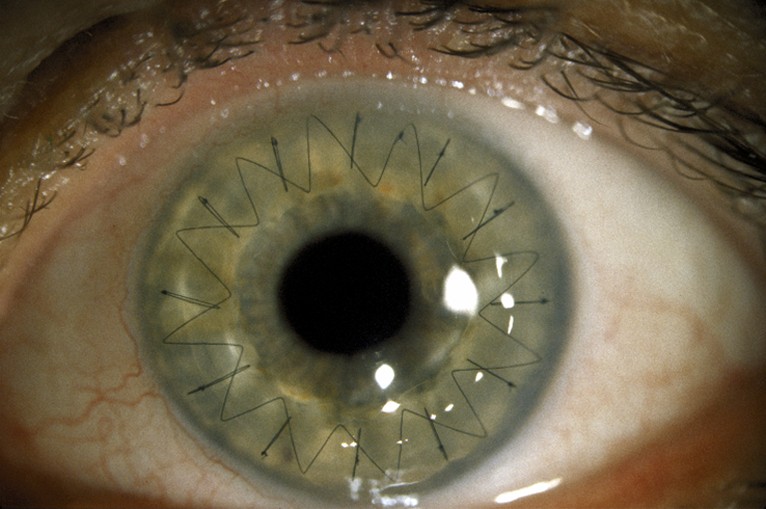
When diagnosed in the early stages, keratoconus may be corrected with eyeglasses, which may require frequent changes in the astigmatism prescription. When the disease is progressing, some patients may benefit from a procedure called; corneal crosslinking. This is a procedure that uses riboflavin and UV light to strengthen collagen bonds, in an attempt to minimize further protrusion of the cornea. As the disease advances, contact lenses usually are necessary to provide clear vision, most often in the form of a rigid gas permeable (RGP) material. Specialized designs of contact lenses are available and are constantly being improved, allowing for fitting of more advanced cases of keratoconus. If there is severe scarring of the cornea and contact lens wear is not possible or does not provide adequate vision, a corneal transplant is needed. This occurs in approximately 20% of patients. A corneal transplant replaces a diseased cornea with a normal cornea from a deceased donor. Most people who receive corneal transplants see very clearly after the surgery. Success rates of corneal transplantation in keratoconus are higher than 90%. While the surgical transplantation of a new cornea will resolve the problem of scarring in a cornea, eyeglasses or contact lenses are usually needed for vision correction after surgery. Due to the irregular shape of the cornea following transplantation, soft contact lenses seldom provide satisfactory vision.
A corneal and contact lens specialist must decide when corneal transplantation is the best recommendation for a specific patient. This is often not a simple, straight-forward decision. Many factors must be considered and balanced, including the patient’s functional needs, the long recovery period (possibly up to one year) and the risk of complications. Very careful contact lens fittings are often attempted before recommending a corneal transplant. One study found that 69% of patients, most of whom were being referred for surgery, could be successfully fit with contact lenses using special designs. Therefore, prior to making the decision to proceed to surgery, every effort should be made to optimally fit a patient with contact lenses, especially if there is not significant corneal scarring affecting vision.
With the proper treatment (glasses, contact lenses or a corneal transplant), most people with keratoconus will enjoy good vision throughout their lives. With modern contact lenses and surgical techniques, it is rare for someone with keratoconus to be severely visually disabled.